Abstract
Background: Granulocyte transfusion (GTX) have been used to prevent or treat life-threatening infection in patients with severe neutropenia, especially after allogeneic hematopoietic stem cell transplantation (allo-HSCT). However, there remains the paucity of data about clinical benefit of GTX after allo-HSCT.
Material and methods: We retrospectively analyzed the transplant outcomes of allo-HSCT patients who underwent GTX in our institution between 2012 and 2016. Overall survival (OS) was estimated by Kaplan-Meier and were compared using the log-rank method. The cumulative incidences of neutrophil engraftment, non-relapse mortality (NRM), relapse, and acute graft-versus-host disease (aGVHD) were evaluated using Gray's method. Pearson's correlation coefficient was used to analysis relationship between transfused granulocyte cells and absolute white blood cells (WBC) increment.
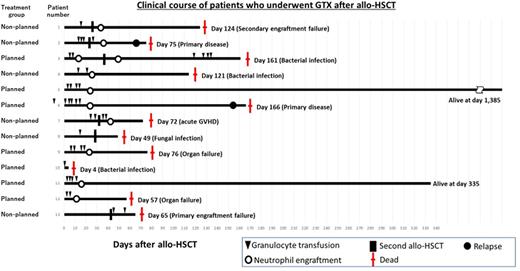
Results: A total of 13 patients received 40 times GTX after allo-HSCT. Median interval between allo-HSCT and the first GTX was 10.5 (range, -8 to 80) days. Seven patients who had infection prior allo-HSCT were received GTX as a planned strategy (planned-GXT group) and 6 patients who suffered from infection after allo-HSCT were treated with GTX (non-planned GXT group). Median age of patients was 58 (range, 30-68) and the underlying disease was predominantly acute myeloid leukemia. Average number of transfused granulocyte was 0.70 (range, 0.10 - 1.61) x 109/kg and median transfusion per patient was 2 (range, 1-6). Median WBC increment one day after GTX was 515 (range, 20-5,090)/μl and WBC increment was significantly correlated with infused granulocyte dosage (p = 0.0054). Average C-reactive protein at GTX and one day after GTX were 11.36mg/dl and 11.01mg/dl, respectively. Neutrophil engraftment rate at 60 days after allo-HSCT was 53.8%. Overall survival (OS) at day 28 and 1 year after GTX were 84.6% and 15.4%, respectively. The incidence of 1-year NRM, 1- year CIR, grade II to IV aGVHD, and grade III to IV aGVHD were 69%, 15%, 39%, and 31%, respectively. Regarding survival, the planned GTX group showed relatively higher OS than the non-planned GTX group (1-y OS, planned GTX group vs. non-planned GXT group, 28.6% vs. 0%, p = 0.062). Infection was the leading cause of death (n = 4), but no patient died by primary infection during neutropenia. Engraftment failure (n =2), organ failure (n = 2), recurrence of underlying disease (n = 2) and acute graft-versus-host disease (n = 1) were followed.
Conclusions:
Successful WBC increment by GTX might prevent to progress infection during neutropenia period without severe adverse event. Patients with uncontrolled infection before allo-HSCT could get the benefits from GTX as a planned strategy. GTX provide the chance for patients with prior history or active infection to receive allo-HSCT.
Nishimori: Toko Pharmaceutical Industries: Other: Investigational drug is provided free of charge.. Maeda: Toko Pharmaceutical Industries: Other: Investigational drug is provided free of charge.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal